Opioid Facts
Three proven and effective strategies are attributed to the prevention and reduction of opioid misuse in NH. These are strategies anyone can do to prevent opioid misuse, overdose and addiction. They are:
When healthcare providers, patients and others work together to support these efforts everyone benefits. Each strategy helps reduce the likelihood of an individual becoming dependent on opioids and reduces the overall access and availability of medication in the community. These strategies work together along with other efforts like education and awareness, coalition building, prescription drug monitoring program and law enforcement.
 Pain is real and can seriously impact the quality of your life. How you manage your pain is important to think about because these choices can also impact your health and well-being.
Pain is real and can seriously impact the quality of your life. How you manage your pain is important to think about because these choices can also impact your health and well-being.
Working with your healthcare provider to create a plan on how to manage your pain begins with:
- Knowing your options – Ask your doctor questions about what other options are available that are often very effective and carry less risk for addiction or overdose. Here are TIPS for starting the conversation with your doctor.
- Consider alternative ways to manage your pain that do not include opioids. Medication is not the only way to manage pain.
- Explore other strategies like chiropractic treatments, physical therapy, acupuncture, and massage to get to the root cause of the pain.
- Join a chronic pain self-management program if you suffer from chronic pain. In NH you can sign up for an in-person or virtual Living Well with Chronic Pain workshop through the UNH Cooperative Extension or Southern NH Area Health Education Center.
No matter what technique you use to manage your chronic pain, having support, a plan of action and information from trusted people and resources can help build your confidence and success. Watch this video to learn how the Living Well with Chronic Pain Program is helping people across NH deal with their pain.
- Discuss with your doctor, the risks for opioid prescriptions.
- Share your concerns about any past experiences with dependency on medication or other drugs, including alcohol.
- Learn about all the side effects.
- Check to see if the medication contains opioids.
- Learn how to reduce the risk of addiction. Physical dependence can occur after only a few days.
Monitor your use and know the signs of potential misuse/ overuse. If you suspect you or someone you love is misusing or overusing a prescription opioid medication, talk to the person’s doctor right away.
Safe use, storage and disposal of prescriptions
 It is important to use, store and dispose of prescription pain medication safely to prevent opioid misuse.
It is important to use, store and dispose of prescription pain medication safely to prevent opioid misuse.
Tips on Safe Use
- Never take prescription opioids in greater amounts or more often than prescribed.
- Always let your doctor know about any side effects or concerns you may have about using opioids.
- Avoid taking opioids with alcohol and other substances or medications. It is very dangerous to combine opioids with other drugs, especially those that cause drowsiness like:
- Benzodiazepines (such as Xanax® and Valium®)
- Muscle relaxants (such as Soma® or Flexeril®)
- Hypnotics (such as Ambien® or Lunesta®)
- Other prescription opioids
- Do not share or sell your prescription opioids.
Tips on Safe Storage
- Put your medication up and away – out of sight. Avoid storing in common areas such as kitchen or bathroom cabinets.
- Store prescription opioids in a secure place, out of reach of others (including children, family, friends, visitors and even pets). Your local Drug Free Community Coalition or Regional Public Health Network may have safe storage containers such as lock boxes to keep your prescriptions safe.
- Keep count of your prescription.
Tips on Safe Disposal
Do not dispose of your unused medication in the garbage or down the toilet. Medicines can pollute water and the environment. Annika Stanley-Smith, Director of Substance Misuse Prevention for the Capital Area Public Health Network, describes the life cycle of a prescription drug, including important steps you can take to prevent putting yourself or others at risk when taking a prescription.
If you have unused prescription opioids at the end of your treatment, you can:
- Reach out to your Regional Public Health Network to find out how to access lock boxes and safe disposal kits and to connect to other resources to prevent substance misuse.
- Dispose of them at a drug takeback center or controlled substance public disposal location in your community any day.
- Dispose of them at a DEA sponsored Drug Take Back Days. They occur two times a year throughout the state.
- Learn how to use household materials to dispose of your medication:
- You can mix your medications with kitty litter or coffee grounds, put them in an airtight container and throw them away.
- You can use a home disposal kit, such as a Deterra bag.
Watch our Safe Medication Storage playlist – This series of videos about how to store, use and dispose of medications in the home were created by the Community Anti-Drug Coalitions of America (CADCA) / AmerisourceBergen Foundation. These videos are for anyone who is looking to learn more about safe practices with medication, particularly parents, caregivers, and grandparents.
Visit Rali NH for more information on efforts to prevent the misuse of prescription medicines around the state.
 Death from an opioid overdose happens when too much of the drug overwhelms the brain and interrupts the body’s natural drive to breathe.
Death from an opioid overdose happens when too much of the drug overwhelms the brain and interrupts the body’s natural drive to breathe.
The following tips can help you or a loved one avoid opioid overdose:
-
- Take medicine as prescribed by your healthcare provider.
- Do not take medication more often than instructed.
- Never mix pain medicines with alcohol, sleeping pills, or illicit substances.
- Never take anyone else’s medication.
- Prevent accidental poisoning by storing your medication out of reach from children and pets. For more information, visit CDC’s Up and Away or Reverse the Silence educational campaigns.
- Dispose of unused medication safely. Your provider can give you information on the safe disposal of unused medications, visit FDA’s drug disposal and DEA’s drug disposal webpages and information on disposal of unused medicines.
What to Do in Case of an Overdose
Opioid overdose is life-threatening and requires immediate medical attention. Call 911 immediately if you see any of the following symptoms in a person:
- Face becomes extremely pale and/or feels clammy to the touch
- Body goes limp
- Fingernails or lips have a purple or blue color
- Vomiting occurs or you hear them making gurgling noises
- Cannot be awakened or are unable to speak
- Breathing or heartbeat slows or stops
It may be hard to tell if a person is “high” or experiencing an overdose. If you aren’t sure, handle the situation like an overdose. By following these steps – you could save a life.
- Call 911 Immediately.
- Give naloxone, if available. Follow the “How to Use” instructions on the product.
- Give rescue breaths, as needed, until person starts breathing or help arrives.
- If person is still not breathing after 2 – 3 minutes of rescue breathing, give another naloxone dose, if available.
- Once the person wakes up, try to keep the person awake and breathing.
- Turn the person on their side to prevent choking.
- Stay with the person until emergency workers arrive.
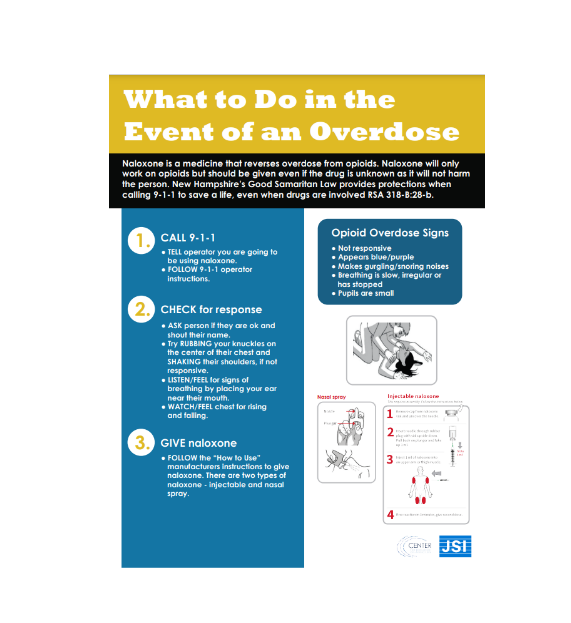 For the latest recommendations, access this visual guide on how to safely respond to an overdose using naloxone (both nasal and injectable) and rescue breathing.
For the latest recommendations, access this visual guide on how to safely respond to an overdose using naloxone (both nasal and injectable) and rescue breathing.
What is Naloxone?
Naloxone is a safe medicine that can quickly stop an opioid overdose. Naloxone can be sprayed into the nose or injected into the muscle of a person to quickly and safely reverse the potential deadly effects of an overdose. Sometimes more than one dose is necessary to get a person to breathe again. You do not need to have a prescription for naloxone and you do not need to be a medical provider to administer naloxone. Naloxone carries no risk of abuse and has no effect on individuals who do not already have opioids in their system. It does not generate physical dependency.
Talk to your doctor about having naloxone on hand if you or a loved one is prescribed opioid medication.
What is Fentanyl?
Fentanyl is an opioid prescribed for people experiencing severe pain due to an injury, surgery, cancer, and to manage pain at the end of life. It is 50 to 100 times more potent than morphine.
What Are Fentanyl Test Strips?
Fentanyl test strips (FTS) are small strips of paper that are used detect the presence of fentanyl. Testing substances with a FTS will tell you if the drug contains fentanyl. FTS are very accurate.
FTS do not:
- Tell you how much fentanyl is in the substance
- Tell if you non-fentanyl drugs are in the substance
Where Can I Get Naloxone or Fentanyl Test Strips?
In New Hampshire, these are available through a number of ways:
- Many pharmacies throughout the state provide naloxone without a prescription.
- The Doorway-NH provides free naloxone and fentanyl test strips and helps with accessing every level of treatment. To find a local Doorway in your area, visit The Doorway.
- Dial 2-1-1: Call 211 or visit thedoorway.nh.gov to get fentanyl test strips and naloxone.
- Many pharmacies throughout the state provide naloxone without a prescription.
- Ask your doctor to write a prescription for the medication for you or a loved one.